Retinal eye diseases are common eye conditions. But, if left untreated for a prolonged time, it can cause trouble. Various retinal diseases i.e. Diabetic retinopathy, vascular diseases, swelling, and detachment are managed in our hospital.
FAQs
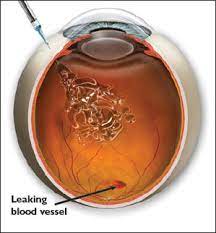
Diabetes affects the retina and this condition is called diabetic retinopathy. It is a microangiopathy affecting the retinal blood vessels. The main features of diabetic retinopathy are microvascular (small blood vessel) occlusion and leakage. As a result of this, there is reduced blood supply to the retina. Due to leaking blood vessels, hemorrhages, and fluid accumulation in the retina can occur.
This initial stage is also called Non-Proliferative Diabetic Retinopathy (NPDR).
As a result of reduced blood supply to the eye because of diabetes, the eye will start forming its own new blood vessels Proliferative Diabetic Retinopathy (PDR), which are fragile hence they can rupture and bleed at any time which leads to sudden drop in vision. This is known as Vitreous hemorrhage. Sometimes in more severe forms traction on the retina can develop that can lead to retinal detachment. This requires treatment in the form of a laser to the eye or surgery or both.
The treatment is to stabilize the patient’s vision and prevent further progression of visual loss.
Proliferative Diabetic
Retinopathy
Diabetic maculopathy is the most common cause of visual loss in diabetic patients. Fluid accumulation leads to swelling in the macula which is the area concerned with vision. It may be focal, diffuse, or ischemic. Focal-focal leakage from the microaneurysms leads to localized swelling.
Diffuse-diffuse leakage which leads to swelling throughout the posterior pole. Ischemic, in this type the blood supply to the macula decreases and this leads to poor vision.
Diabetic Maculopathy
Lasered Retinopathy
Fundus Fluorescein Angiography (FFA) and Optical Coherence Tomography (OCT) are the two investigative procedures that may be done before the treatment plan for Diabetic Retinopathy.
Fundus Fluorescein Angiography (FFA)
This is a diagnostic procedure where fluorescein dye is injected into a vein of the hand and then a series of photographs of the patient’s retina are taken. This gives us a picture of the passage of the dye through the microvasculature of the eye. This helps us to know the status of the blood vessels in the retina and reveals blockage and excess leakage of the dye in case of abnormal new blood vessels.
It also helps us to know whether the patient needs laser photocoagulation or not.
The treatment is usually in the form of a laser or rarely an injection is given in the eye. The laser treatment may be done in 1- 3 sittings
Every patient once diagnosed to have diabetes should have regular eye check ups every 6 months.
Macula (central retina) – appreciation of fine details, reading and color vision. Peripheral retina – functions for night vision
Sudden or gradual decrease in vision
Loss of field of vision
Flashes of light
Floaters
Objects appearing distorted (Metamorphopsia)
Night Blindness
Whenever a patient has any of the above-mentioned symptoms he is advised to have an immediate check-up with a retina specialist.
Regular eye examinations if the patient is diabetic, hypertensive, and over forty years old.
Common diseases include
Diabetes mellitus
Hypertension
Age-related macular degeneration
Myopia
Infectious diseases
Hereditary degeneration
Congenital degeneration
Rarely drugs used for some systemic diseases affect the retina
You may sometimes see small specks or clouds moving in your field of vision. They are called floaters. You can often see them when looking at a plain background, like a blank wall or blue sky. While these objects look like they are in front of your eye, they are actually floating inside. What you see are the shadows they cast on the retina. Floaters can have different shapes: little dots, threads, circles, lines, clouds, or cobwebs.
When people reach middle age, the vitreous gel may start to shrink, forming clumps or strands inside the eye.
Posterior vitreous detachment (PVD): The vitreous gel pulls away from the retina, causing a posterior vitreous detachment. It is a common cause of floaters.
PVD is more common for people who:
are shortsighted or myopes ;
have undergone cataract operations;
have had YAG laser of the eye;
have had inflammation inside the eye / any trauma
Infectious diseases
Hereditary degeneration
Congenital degeneration
Rarely drugs used for some systemic diseases affect the retina
The retina can tear if the shrinking vitreous gel pulls away from the retina. This sometimes causes a small amount of bleeding in the eye that may appear as new floaters.
A torn retina is always a serious problem since it can lead to a retinal detachment. You should see your retina specialist as soon as possible if even one new floater appears suddenly or you see sudden flashes of light or if you notice other symptoms like the loss of side vision.
Floaters can get in the way of clear vision, which may be quite annoying, especially if you are trying to read. You can try moving your eyes, looking up and then down to move the floaters out of the way.
While some floaters may remain in your vision, many of them will fade over time and become less bothersome. Once your retina is examined and everything is normal, you can ignore the floaters.
When the vitreous gel rubs or pulls on the retina, you may see what looks like flashing lights or lightning streaks. You may have experienced this same sensation if you have ever been hit in the eye and seen “stars.”
The flashes of light can appear off and on for several weeks or months. As we grow older, it is more common to experience flashes. If you notice the sudden appearance of light flashes, you should visit your Retina specialist immediately to see if the retina has any problem.
If the tear has not caused a retinal detachment(RD) then a laser is done surrounding the hole/tear to seal it. This reduces the risk of RD. However, you need to regularly follow up with a retina specialist as new holes/tears can still form.
Myopia is also known as short-sightedness. It is a disorder in which a person cannot focus on distant things clearly.
The light rays from an object are focused in front of the retina, making them look blurred.
It is corrected with minus numbered lenses / Lasik surgery.
Myopia can affect the retina in the following ways.
Myopes have larger eyeballs and can develop retinal thinning and degeneration in the peripheral parts of the retina, these occur due to stretching of the globe.
These degenerations are prone to progress and later may form holes or tears in the retina.
These retinal holes or tears if not treated can lead to retinal detachment, which will cause sudden loss of vision and will require major surgery at the earliest, to prevent further loss of vision.
Sometimes the central part of the retina (macula) may be affected by macular degeneration or choroidal neovascular membrane.
Affects people usually over 60 years of age and is a leading cause of blindness in elderly people
Distortion of lines or objects
(Alphabets appear distorted or wavy while reading) Cloudiness or decrease in
central vision. Decrease in color vision
Dry-type (drusen)
The most common cause of vision loss in old age is visual loss is usually gradual. This occurs due to the accumulation of a specific material in the aging cells in the macula as a result of this the cells do not work normally and vision becomes blurred.
Treatment:
Some patients benefit from systemic antioxidant or macronutrient vitamins for the retina.
Wet Type (choroidal neovascular Membrane)
This occurs in 10-15% of patients with ARMD but the loss of vision is more profound and may also be sudden sometimes.
This occurs due to the formation of a membrane or layer of new blood vessels called Choroidal neovascular membrane (CNVM) which occurs beneath the retina. These new blood vessels can leak blood or fluid that leads to loss of vision and distortion.
Treatment initiated at the earliest stabilizes the vision.
Various modes of treatment include:
Laser photocoagulation
Photodynamic therapy (PDT)
Intravitreal injection of Anti-VEGF drugs( Lucentis Macugen or Avastin)
Combination therapy or monotherapy will be decided by the retinal specialist.
Usually, a Combination therapy of any two of the above is done.
Wet Macular Degeneration
Photodynamic therapy is performed by injecting a special dye known as Verteporfin. Intravenous verteporfin selectively localizes in new blood vessels and is activated by laser light on the target area. Nonthermal laser energy (diode laser, operating at a wavelength of 689 nm) is then applied locally to the CNVM to produce photochemical reactions that lead to the closure of a new vessel (thrombosis).
More than one treatment session may be required to achieve complete closure.
Lucentis ( Ranibizumab)
Avastin (Bevacizumab)
Macugen (Pegaptanib sodium)
Lucentis /Macugen /Avastin:
These are the latest drugs that have given a ray of hope to improve vision in patients with wet ARMD. These are drugs that prevent the formation of new blood vessels and reduce leakage.
More than one injection may be necessary.

