Squint Management
Squint (भेंगापन) is a disease due to the misalignment of eye muscles. This may occur in infants & older children as well as in adults. Various treatment modalities ( medicines, spectacles, exercises & surgery ) are used to treat this disease. We provide services like Comprehensive preschool check-ups, ROP screening, Glasses prescription, Lazy eye Screening, and Screening for special children with a special squint clinic in operation. Apart from this, the surgical procedures for squint treatment can also be consulted at A.H.E.C that too with proper machinery, and an expert team.
FAQs
Take a good look at your child while he/she is playing or watching a book/TV and note if any of the following are present.
• Squeezing his/her eyes while looking at books/Tv/Toys.
• Tilting the head while talking, walking/ playing.
• Going too close to the book or TV.
• Recurrent eye pains, headaches.
• Avoids reading, and colouring most of the time.
• Has bad handwriting at school.
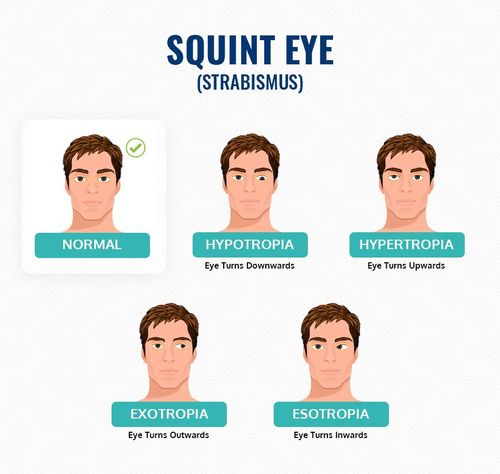
• Eyes turning inwards/outwards.
• Difficulty in seeing in sunlight, bright light in the evening.
• Itching, watering.
If any of the above are present then you should suspect the child to have a possibility of eye problem. The problem could be either glasses or squinting of the eyes. These are easily treated and a proper screening of the child having any of the above complaints is needed to rule out any other causes as well.
All children should be seen by an eye doctor for the first time at 3-4 years of age However if any of the following are present then the child should be brought to the eye doctor at the earliest:
• One on both parents wearing glasses
• History of consanguinity(marriage among cousins) in family
• Premature delivery
• Birth weight less than 1.5 Kg.
• History of any congenital defects like heart, kidney, etc.
• History of febrile fits or any convulsion.
• History of admission in the ICU- incubation/ ventilation given to the child.
• Behavioural disorders or any developmental delay in the child.
• History of color blindness and retinal disease in the family.
• Early detection of eyesight problems gives rise to better vision development.
• Good vision correction causes good performance at school and home.
• Squinting of an eye if diagnosed early can be treated with exercises and glasses in some cases.
• It is possible to give the child good binocular(coordinated) development of eyes.
• Other behavioral, and social problems if present in the child will also benefit from their treatment.
If the child has a problem then any time is a good time to visit the eye doctor however specific visits can be planned as follows
• A preterm infant/low birth at infant at 4 weeks after birth.
• A normal baby at 3 to 3½ years of age for a preschool eye check.
• Comprehensive preschool checkup
• Watery eye evaluation
• ROP screening
• Squint clinic
• Glasses prescription
• Lazy eye Screening
• Visual disorders management
• Screening for special children
This involves a complete screening of a child for vision, squint, retina, and optic nerve disorders. For preschool eye checks following examinations are carried out
• Examination of the anterior part of the eye: screening for congenital corneal disease, anterior chamber, and lens diseases.
• Vision testing: the ability of the child to see, which is measured by specialized preschool picture charts of international standards and is age-matched.
• Examination of the presence of any deviation or squinting of the eyes: this is carried out by special measuring instruments that are child-friendly and not intimidating to the child in any way.
• Binocular vision function of eyes testing: here the tests are performed to ascertain whether there is coordinated use of both eyes.
• Color vision, pupil, and contrast sensitivity testing.
• Examination of the intraocular pressure: this is done in children, especially with a positive family history or examination findings suggestive of an increase.
• Check for confirmation of eyeglasses power: by special eye drops after relaxing the eye muscles so that any glass power that is hidden and not apparent can also be screened
• Examination of the retina and optic nerve.
Medical
• Lazy eye management.
• Glass prescription.
• Eye exercises.
• Low vision aids.
• Allergic eye conditions.
• Eye infections.
• Glaucoma management.
• Retinal lasers.
Surgical
• Congenital cataract management.
• Glaucoma surgeries.
• Corneal transplant.
• Squint correction.
• Pediatric Lasik.
• Retinal surgeries in children.
PTERYGIUM
A pterygium is a pinkish, triangular-shaped tissue growth on the cornea. Some pterygia grow slowly throughout a person’s life, while others stop growing after a certain point. A pterygium rarely grows so large that it begins to cover the pupil of the eye.
Pterygia are more common in sunny climates and in the 20-40 age group. Scientists do not know what causes pterygia to develop. However, since people who have pterygia usually spend a significant time outdoors, many doctors believe ultraviolet (UV) light from the sun may be a factor. In areas where sunlight is strong, wearing protective eyeglasses, sunglasses, and/or hats with brims is suggested. Because a pterygium is visible, many people want to have it removed for cosmetic reasons. It is usually not too noticeable unless it becomes red and swollen from dust or air pollutants.
Pterygium excision is not recommended unless it affects vision. If a pterygium is surgically removed, it may grow back, particularly if the patient is less than 40 years of age. Lubricants can reduce the redness and provide relief from chronic irritation.
Pterygium Surgery with Grafting
In addition to other surgeries, we at Anand Eye Hospital also offer Pterygium surgery with grafting to our entire patients as we are a renowned eye hospital in Jaipur (Rajasthan). Pterygium surgery with grafting offered by Anand Eye Hospital is one of the best and most effective surgical procedures for the eyes. Being a very client-oriented organization; we offer Anand Eye Hospital’s Pterygium surgery with grafting at very reasonable charges.
• No-stitch pterygium surgery USING GLUE is made possible by the use of modern tissue adhesive*, composed of clotting proteins normally found in human blood. Tissue adhesive allows the surgeon to secure a conjunctival autograft in seconds rather than minutes. After about one week the tissue adhesive dissolves, leaving no residue, and the eye heals comfortably.
UV radiation (usually from sunlight) is the most common cause of pterygium. This explains why pterygium occurs with increasing frequency in climates approaching the equator. Other causes include continuous exposure to dry, dusty environments. People who spend significant time in water sports (surfing or fishing) are particularly susceptible to pterygium because of the intense exposure to UV that occurs in these environments. When the eye is continuously assaulted by UV rays, the conjunctiva may thicken in a process similar to callus formation on the skin. The sensitive structures of the outer eye often can not comfortably tolerate this degenerative process, and irritation, redness, foreign body sensation, and ocular fatigue can result.
In mild cases, pterygium redness and discomfort can be controlled with lubricant eye drops (artificial tears). When symptoms of redness, irritation, or blurred vision are resistant to conservative treatment, or when vision is affected by progressive growth of a pterygium, surgery is considered.
In pterygium surgery, the abnormal tissue is removed from the cornea and sclera (white of the eye). Over the years, pterygium surgery has evolved significantly, and modern pterygium surgery has a significantly higher success rate than conventional surgery.
In traditional “bare sclera” pterygium removal, the underlying white of the eye (sclera) is left exposed. Healing occurs over two to four weeks with mild to moderate discomfort. Unfortunately, the pterygium may grow back in up to 50% of patients. In many cases, the pterygium grows back larger than its original size.
Traditional “bare sclera” pterygium surgery has a high rate of re-growth. Occasionally, the pterygium grows back larger than the original.
Over the years, surgeons have used several different techniques to lessen the likelihood of pterygium recurrence, including radiation treatment and the use of “antimetabolite” chemicals that prevent growth of tissue. Each of these techniques has risks that potentially threaten the health of the eye after surgery, including persistent epithelial defects (ulceration in the surface of the eye), and corneal melting.
Most cornea specialists today perform pterygium surgery with a conjunctival autograft because of a reduced risk of recurrence. In this technique, the pterygium is removed, and the cornea regains clarity. However, the gap in the mucous membrane (conjunctiva) tissue, where the pterygium was removed, is filled with a transplant of tissue that has been painlessly removed from underneath the upper eyelid. Although the procedure requires more surgical skill than traditional surgery, this “auto-graft” (self-transplant) helps prevent re-growth of the pterygium by filling the space where abnormal tissue would have re-grown.
In conventional autograft surgery, stitches are used to secure the graft in place on the eye. These can cause discomfort for several weeks.
The autograft is held in place with tiny stitches that may dissolve after a few weeks or can be removed in the surgeon’s office. Stitches on the eye frequently cause discomfort, however, after pterygium/autograft surgery. The desire for a quicker, more painless recovery has led to the development of no-stitch pterygium/autograft surgery.
• No-stitch Pterygium/Autograft Surgery with Glue
• No-stitch pterygium/autograft surgery allows most patients to return to work the next day of surgery. The no-stitch technique also reduced surgery time from an average of 21 minutes to 14 minutes. No pterygium recurrences were found in most of the patients
• Technique for No-stitch Pterygium/Autograft Surgery
• In no-stitch surgery, after local anaestheisia there is no sensation of discomfort. The abnormal corneal tissue is removed and replaced with a thin graft of normal tissue using high definition and tissue friendy Glue . Over the next 1 week, the eye gradually returns to a normal appearance.

